Deep-learning tech reveals personal ID of cancer cells
Just as every handwritten signature is unique, so is every cancerous tumor. Researchers at the Technion-Israel Institute of Technology have now used artificial intelligence and big datato decode the unique signatures of certain cancer cells.
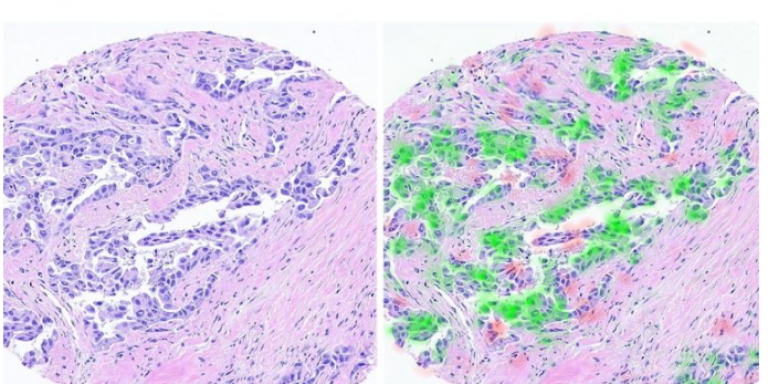
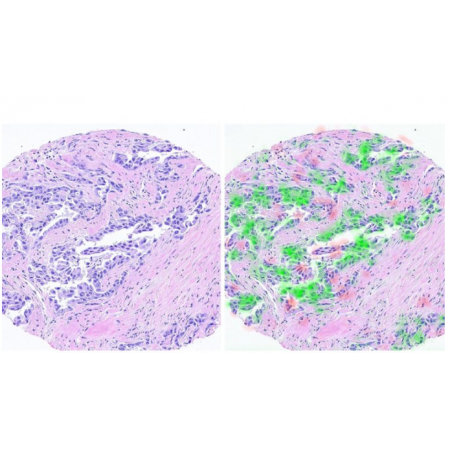
Technion’s computerized pathologist decodes cancer signatures to improve personalized medicine.
The resulting technology – dubbed a “computerized pathologist” –could significantly boost development of personalized cancer treatments.
The researchers worked with digital images from breast-cancer biopsy samples. The new technology, described earlier this summer in the medical journal JAMA, extracts molecular information from the cell shape (morphology) and its environment.
“Pathologists we spoke to said it was an impossible task,” explained doctoral student Gil Shamai, who worked with Prof. Ron Kimmel of the Technion’s Faculty of Computer Science and fellow doctoral student Ron Slossberg.
“A human pathologist cannot infer the tumor features from its shape because of the sheer number of variables. The good news is that artificial intelligence technologies, and especially deep learning, are capable of doing so. The computer, unlike even the most skilled pathologist, can characterize the cancer with a complex analysis of its morphology.”
With the help of image processing and AI tools, the researchers predicted the molecular profile of cancerous cells just by looking at the tissue as it appears on standard biopsy scans.
“We succeeded in identifying the ‘signature’ that the cancer leaves in the tissue,” Shamai added.
The team had to write its own software code to compare the biopsies it was analyzing with samples of more than 20,000 scans from 5,356 breast cancer patients. Such deep learning systems “require a huge amount of information and obtaining the kind of information required is not easy.”
The researchers were then able to map estrogen and progesterone receptors along with other molecular biomarkers. The study focused on breast cancer, but the technology will be relevant to all cancers.
“This is a feasibility study,” said Kimmel. “In the first phase, we believe it will be a tool to help doctors make decisions and will later be developed as a real clinical tool.”
The research was supported by the Ministry of Science and Technology, the National Science Foundation, the Lorry Lokey Interdisciplinary Center for Life Sciences and Engineering, and Schmidt Futures. Dr. Yoav Binenbaum of Tel Aviv Medical Center and Prof. Ziv Gil of Rambam Medical Center also participated in developing the technology.